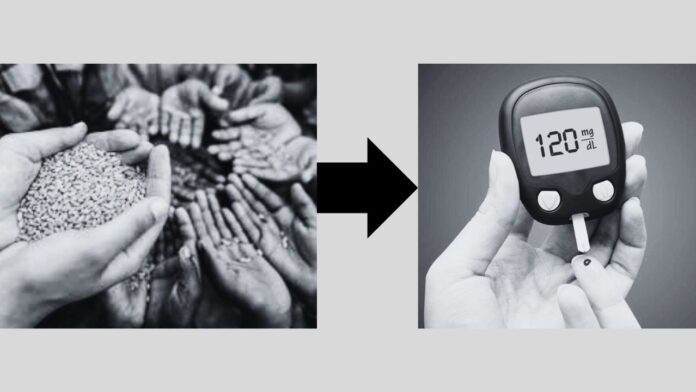
The history of British rule in India is marred by exploitation, oppression, and policies that led to catastrophic famines. Recent studies have highlighted a grim legacy of these famines: the genetic and epigenetic alterations in the South Asian population that have contributed to the current diabetes epidemic. This article delves into the historical context, the scientific basis of these genetic changes, and the present-day implications for millions of people in India, Pakistan, and Bangladesh.
Historical Context: British Rule and Famine
British colonial rule in India, which lasted from 1757 to 1947, was characterized by economic policies that prioritized British interests over the welfare of the local population. During the British Raj (1858-1947), India experienced 25 major famines, resulting in the deaths of at least six million people. In stark contrast, only 17 major famines were recorded in the two thousand years preceding British rule.
Several factors contributed to these famines, including the British highland tax, reduced spending power of Indian subjects, and the export of domestically produced food to Britain. The Bengal Famine of 1943, which resulted in the deaths of over three million people, exemplifies the devastating impact of these policies. During World War II, large quantities of commodities were exported from India, exacerbating the food crisis and leading to widespread malnutrition and starvation.
The Epigenetic Legacy of Famine
The concept of epigenetics provides insight into how environmental factors, such as famine, influence the expression of genes across generations. Epigenetic modifications do not change the DNA sequence itself but can alter how genes are expressed. These changes can be passed down from one generation to the next, affecting how the body responds to various stimuli, including food.
During the British-imposed famines, the bodies of those who survived adapted to the severe scarcity of food. These adaptations, known as “starvation adaptations” or “famine tolerance,” resulted in increased insulin resistance—a condition where the body’s cells become less responsive to insulin. Insulin is a crucial hormone that helps process food and regulate blood sugar levels. Insulin resistance can lead to higher blood sugar levels, a hallmark of type 2 diabetes.
The Present-Day Diabetes Epidemic
Today, South Asia has one of the highest rates of type 2 diabetes in the world, with prevalence six times higher than in Europe. The epigenetic changes from the famine era have left the population predisposed to insulin resistance. As a result, even minor disruptions in diet and lifestyle can significantly increase the risk of diabetes.
The modern food environment exacerbates this problem. Processed and packaged foods, which often contain added sugars, dominate diets worldwide. In South Asia, where traditional diets have been replaced or supplemented with these high-sugar, high-fat foods, the consequences are severe. The combination of genetic predisposition and unhealthy food choices has led to skyrocketing rates of diabetes, obesity, and related health issues.
The Role of Lifestyle and Diet
Historically, South Asian cultures had sophisticated medical and physical practices, such as Ayurveda and Yoga, which promoted health and well-being. These practices, coupled with a traditional diet rich in whole foods, helped maintain metabolic health. However, the shift to a more Westernized diet and sedentary lifestyle has disrupted this balance.
Reversing the tide of diabetes in South Asia requires a return to these traditional practices. Emphasizing whole foods, reducing the intake of processed foods, and incorporating regular physical activity can help mitigate the effects of the genetic predisposition to insulin resistance.
Conclusion: Decolonizing Medical Research and Health Practices
The Guardian’s report underscores the need to decolonize medical research and health practices. Understanding the historical context of health issues in South Asia is crucial for developing effective interventions. This includes acknowledging the long-lasting impact of British colonial policies on the region’s health and addressing the epigenetic changes that continue to affect millions.
By promoting lifestyle and dietary changes rooted in traditional practices, it is possible to reduce the risk of type 2 diabetes. While the genetic legacy of famine cannot be erased, its impact can be mitigated through informed and culturally appropriate health strategies.
In conclusion, the diabetes epidemic in South Asia is not merely a consequence of modern lifestyle choices but a complex interplay of historical, genetic, and environmental factors. Recognizing the colonial legacy and its epigenetic repercussions is essential for addressing the current health crisis. Through a combination of decolonized medical research, traditional health practices, and modern science, it is possible to chart a path towards better health outcomes for future generations in South Asia.